As more people aged 45-49 are getting screened for colon cancer, more early stage diagnoses are being made, according to new research from the American Cancer Society.
The research, published in two studies Monday in the Journal of the American Medical Association, showed increases in screenings among those younger than 50 is linked to rises in earlier diagnosis. One study showed an annual increase of 1.1% from 2004 to 2019 jumped to 12% from 2019 to 2022 for colorectal cancer incidence among people aged 45 to 49, while another study showed screenings among U.S. adults aged 45 to 49 increase 62% from 2019 to 2023.
The recommended age to begin colorectal screening was lowered from 50 to 45 by the ACS in 2018 and by the U.S. Preventive Services Task Force in 2021.
In a news release Monday, Elizabeth Schafer, lead author and surveillance and health equity scientist, called the findings "promising news."
"The uptick of cases is likely due to first-time screening in the wake of new recommendations for younger average-risk adults to begin testing for colorectal cancer earlier," Schafer explained.
Another lead author, Jessica Star, who does cancer risk factors and screening surveillance research at the ACS, said it's "thrilling" to see increases in screening rates among younger adults as well as its likely ties into rises in earlier stage diagnosis.
Still, she warned there's a long way to go.
"Screening for colorectal caner in ages 45-49 remains suboptimal and has not increased equitably by both education attainment and insurance status," Star said in the release.
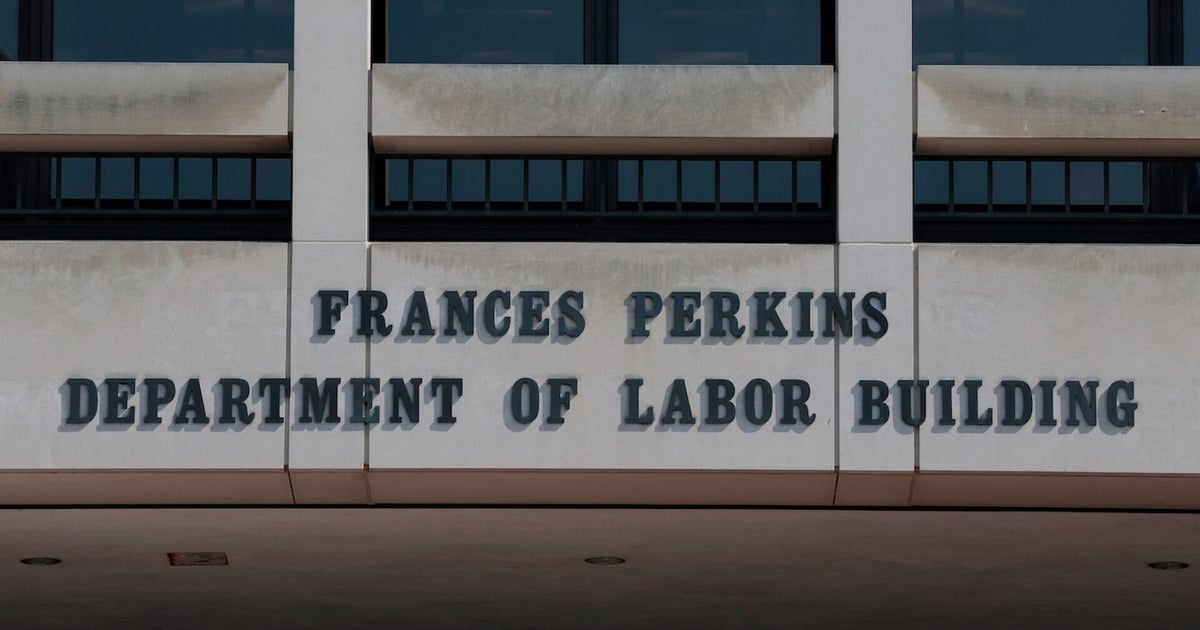
Recently, medical associations expressed concern after a report that Health and Human Services Secretary Robert F. Kennedy may remove all members of the U.S. Preventive Services Task Force, a panel of independent medical experts whose recommendations help guide insurance companies and doctors' decisions about a range of preventive health measures, like cancer screenings.
Dr. Thomas Lew, an assistant clinical professor of medicine at the Stanford University School of Medicine and attending physician of hospital medicine at Stanford Health Care Tri-Valley, recently told CBS News that a change like this would "greatly damage all the work we've done in preventative care, making people sicker, and driving up costs and premiums."
"To put it mildly, this is extremely concerning — and doing the opposite of making America healthy," Lew said.
In a statement to CBS News at the time, an HHS spokesperson said, "No final decision has been made on how the USPSTF can better support HHS' mandate to Make America Healthy Again."
Sara Moniuszko